How Does Your Health Insurance Plan Stack Up? There’s A Resource for That
/Connecticut’s Insurance Department has issued its 2018 Consumer Report Card on Health Plans in Connecticut, providing consumers with an updated snapshot of 12 health carriers in the Connecticut marketplace. The goal: to help consumers make informed choices when choosing a health plan.
“The Department’s annual Report Card is designed to deliver side-by-side comparisons of health carriers across a variety of quality measures, including coverage for mental health and substance abuse treatment,” Commissioner Katharine L. Wade said recently. The analysis includes health claims, mental healthcare, pregnancy coverage and preventative care, and reviews the reasons cited in instances of denial of coverage. 
Among the trends identified in the latest annual report care are:
- Total enrollment over 2.2 million, a slight increase from 2016.
- 5 percent of those covered (1.85 million people) get their insurance from large group plans
- 131,000 people have individual plans (5.9 percent)
- 235,000 people are covered under small group plans (10.6 percent)
The 72-page data-filled report card also notes that there was an increase in the number of primary care providers, specialists and pharmacies participating in health plan networks. There was a decline in the number of participating hospitals, officials indicated, but attributed it “primarily due to consolidations in the industry and not facilities closing.”
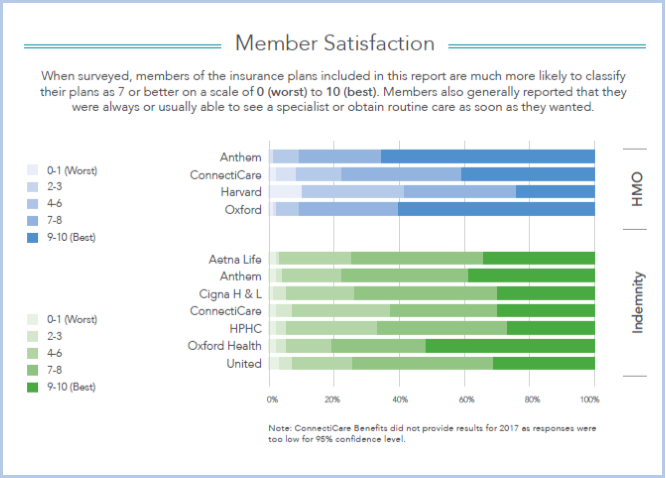
Customers surveyed said they were always or usually able to see a specialist or get routine care as soon as they wanted. The enrollment breakdown in Connecticut is lopsided. Among HMO's, Anthem has 81% of the market, ConnectiCare 17%, Oxford 2%. Among indemnity enrollments, Anthem has 42%, followed by Aetna's 20%, CIGNA's 19%, United's 7% and ConnectiCare's 5%.
The report card, issued this fall, includes “terms” that consumers should know, a series of frequently asked questions and answers, and results of a member satisfaction survey for HMO’s Anthem, ConnectiCare, Harvard Pilgrim and Oxford Health. Indemnity insurers Aetna Life, Anthem, CIGNA, ConnectiCare, Harvard Pilgrim, United Health and Oxford Health also had members surveyed on a range of “satisfaction” queries.
This report includes three years of data, where available, to be informative for consumers, officials said. The data utilized was through 2017.
The mission of the Connecticut Insurance Department is to protect consumers through regulation of the industry, outreach, education and advocacy. The Department recovers an average of $4 million yearly on behalf of consumers, according to officials, and regulates the industry by ensuring carriers adhere to state insurance laws and regulations and are financially solvent to pay claims.
Each year, the Department returns an average of $100 million a year to the state General Fund in license fees, premium taxes, fines and other revenue sources to support various state programs, including childhood immunization. The Department’s annual budget is funded through assessments from the insurance industry.
Individuals with questions or seeking further information may contact the Department at insurance@ct.gov or 860-297-3900.