Correctional Institutions or Institutions for the Mentally Ill? Governments Seek New Solutions
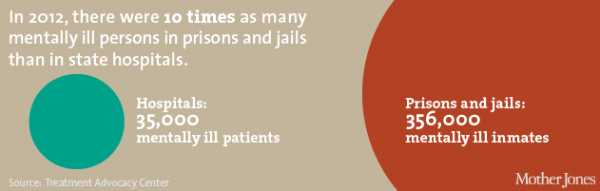
/How to effectively respond to the fact that America’s prisons have rapidly become de facto institutions for the mentally ill is increasingly gaining attention in policy circles and the news media. In recent days, The New York Times, Governing magazine, and other publications have focused both on the alarming statistics and some innovative approaches across the country. There are now 10 times as many mentally ill people in the nation’s 5,000 jails and prisons as there are in state mental institutions, according to a study last year by the National Sheriffs’ Association and the Treatment Advocacy Center, a nonprofit group that supports expanded access to treatment, the Times reported.
In Connecticut, out of the 16,154 inmates in state prisons, about 3,423 have a serious mental illness, 21 percent of the total prison population, Michael Lawlor, undersecretary for criminal justice policy and planning at the Office of Policy and Management, told the New Haven Register earlier this year. Just a few years ago, the National Alliance on Mental Illness (NAMI) estimated that approximately 16 percent of the state’s prison population consisted of persons with mental illness.
The State Department of Correction confirms that those defined as “seriously mentally ill” include 17 percent of the male population, 66 percent of the female population, and 20.8 percent of the overall prison population in the state.
According to the Council of State Governments, jails in the U.S. report that between 20 and 80 percent of their inmates suffer from a mental illness, Governing reported. Today’s acute challenge has been decades in the making. In the mid-1950’s, the publication indicated, more than 500,000 people were held in state psychiatric hospitals. “By the 1980s that number had fallen to around 70,000. During this period, the number of people with mental illnesses who were arrested and ended up in local jails surged.”
Chicago’s Cook County Jail, now referred to by local officials as the nation’s largest mental institution in the country, has 8,600 inmates – an estimated one-third of them suffering from mental illness. The newly appointed warden of the facility is a clinical psychologist – underscoring “how much the country’s prisons have become holding centers for the mentally ill,” the Times reported.
 Writing in the Connecticut Law Review, Christina Canales observed that “Many supported deinstitutionalization because they believed that the mentally ill would benefit from being released from the state hospitals. They believed that with the assistance of anti-psychotic medications, the mentally ill would be able to live independently in the community and that the community mental health centers would provide the additional care, treatment, and follow up services.
Writing in the Connecticut Law Review, Christina Canales observed that “Many supported deinstitutionalization because they believed that the mentally ill would benefit from being released from the state hospitals. They believed that with the assistance of anti-psychotic medications, the mentally ill would be able to live independently in the community and that the community mental health centers would provide the additional care, treatment, and follow up services.
“Although a good plan in theory,” Canales concludes, “deinstitutionalization quickly became one of the main reasons for the substantial increase in mentally ill people in jails and prisons. Patients were ejected from state mental hospitals at a substantially faster rate than community mental health programs were created.”
The Law Review article, published three summers ago, concludes that “the United States faces a crisis in that prisons are among the largest mental healthcare providers. Some mentally ill individuals turned to crime after deinstitutionalization left them on the streets with no support system. Others wound up in prison because police officers lacked the proper training to identify persons as mentally ill and in crisis, or mistakenly believed that individuals receive adequate treatment in prison. The change in civil commitment laws also made it harder to commit the mentally ill, and society as a whole wants these individuals punished, mentally ill or not.”
Earlier this year, the Connecticut state legislature considered – but did not approve - a bill that would have established a pilot program to serve courts in New Haven, New London and Norwich to identify and track the mentally ill, along with homeless and addicted individuals entering the criminal justice system. The idea behind it was to get these individuals treatment and help as an alternative to incarceration and to prevent future arrests, according to published reports. The initiative also called for a formal assessment of its effectiveness.
In Chicago, the Times reported, “before becoming warden, Dr. Nneka Jones Tapia oversaw mental health care at the jail, and under her guidance, Cook County began offering services that would have been unthinkable a few years ago. All inmates upon arrival now see a clinician who collects a mental health history to ensure that anyone who is mentally ill gets a proper diagnosis and receives medication. The jail then forwards that information to judges in time for arraignments in the hope of convincing them that in certain cases, mental health care may be more appropriate than jail.”
According to a report by the Virginia-based Treatment Advocacy Center, 95 percent of the public psychiatric beds available in 1955 in the country were no longer available by 2005, the New Haven Register reported. The Center recommends a minimum of 50 beds per 100,000 people, a standard that no state meets. Connecticut has about 20 public psychiatric beds per 100,000 people, according to the center’s website. Between 1995 and 2013, the number of inpatient psychiatric beds, at both public and private hospitals, decreased from 160,645 to 107,055 nationally, according to data from the American Hospital Association.
Connecticut, which recently approved a Second Chance Society Act proposed by Gov. Malloy that reduces some criminal sentences for nonviolent offenses and drug possession, is expected to reduce the number of people incarcerated for drug use, which officials expect will also reduce the number of mentally ill in prisons, “since drug use and mental health problems frequently coexist in a significant group” of the population.
The Governing article highlights a diversion system in Miami-centered Dade County in Florida, a post-booking alternative program that permits individuals arrested for “misdemeanor offenses and identified as having acute mental illnesses” to be transferred to mental health treatment facilities. The results, according to the publication:
“About 80 percent of people offered the chance to participate in the program accepted it. What was surprising was how many people stayed out of the system afterward. An evaluation conducted soon after the program began found that recidivism rates one year out among participants who complete the program was just 20 percent. In contrast, 72 percent of peers who did not participate in the program were back in jail within one year of their release.”
https://youtu.be/zSbFbv2Bs_0?list=PLQ9B-p5Q-YOP2OVnCPdYKLSmPkqLA2igT


 re available at all prisons and jails in the state, with comprehensive mental health programs at Osborn, Northern, York, Manson Youth, and Garner correctional institutions. Mental health services are comprehensive from admission to discharge, the website explains, and “focus on access to care and outreach, screening and assessment, identification, treatment planning, classification, provision of distinct levels of service and continuity of care upon discharge to the community.”
re available at all prisons and jails in the state, with comprehensive mental health programs at Osborn, Northern, York, Manson Youth, and Garner correctional institutions. Mental health services are comprehensive from admission to discharge, the website explains, and “focus on access to care and outreach, screening and assessment, identification, treatment planning, classification, provision of distinct levels of service and continuity of care upon discharge to the community.” s. Thoughtful release planning and progressive probation or parole procedures increase the likelihood of successful re-entry for prisoners living with mental illness.”
s. Thoughtful release planning and progressive probation or parole procedures increase the likelihood of successful re-entry for prisoners living with mental illness.”