The Indiana Insurance Department will consider the proposed acquisition of Bloomfield-headquartered CIGNA Health Care by Indianapolis-based Anthem, Inc. at a public hearing on Friday, April 29 in Indianapolis. “Any member of the public interested in the proposed acquisition of control may attend the hearing,” indicates a public notice of the hearing. In addition, “Any policyholder of Cigna HealthCare of Indiana, Inc., or other person whose interests may be affected by the proposed acquisition of control shall have the right to appear and become party to the proceeding.”
“Any member of the public interested in the proposed acquisition of control may attend the hearing,” indicates a public notice of the hearing. In addition, “Any policyholder of Cigna HealthCare of Indiana, Inc., or other person whose interests may be affected by the proposed acquisition of control shall have the right to appear and become party to the proceeding.”
Officials indicated that written testimony could be mailed in lieu of an in-person appearance, and would be considered. Members of the public may make written submissions without appearing in person at the hearing. Length of submissions should not exceed 5 pages, double-spaced. Officials indiated that submissions should be sent to John Murphy, outside counsel to the Commissioner in this matter, by close of business on April 26, 2016. Contact information is: John T. Murphy, ICE MILLER LLP, One American Square, Indianapolis, IN 46282, (317) 236-2292, john.murphy@icemiller.com [this information was updated on 4/19]
Consumer Groups, State Comptroller Call for Full Review
Among those aligned in opposition to the acquisition is the American Medical Association, noting that the deal would make the combined firm the nation’s largest insurer by membership and also give the company a tremendous amount of leverage when negotiating with providers. In a press release, AMA President Steven J. Stack, MD, said such proposed mergers threaten to reduce competition and choice. “To give commercial health insurers virtually unlimited power to exert control over an issue as significant and sensitive to patient health care is bad for patients and not good or the nation’s health care system.”
Anthem and CIGNA suggested that the deal will create new efficiencies that will make the healthcare market function more efficiently. A website, www.betterhealthcaretogether.com, has been established to highlight the companies commitment to “drive health care innovation.”
Last month, a coalition of consumer and medical organizations in Connecticut called for greater public input into the Connecticut Insurance Department’s review of the proposed Anthem-CIGNA mega-merger, expressing concerns about the potential “negative impact on both the cost and quality of care in Connecticut” of that acquisition and the proposed Aetna-Humana merger. The groups – Universal Health Care Foundation, Connecticut Citizen Action Group and the Connecticut State Medical Society – formed the “Connecticut Campaign for Consumer Choice” coalition and urged state Insurance Commissioner Katherine Wade to “ensure an open, transparent hearing process in Connecticut, where policy holders, physicians and other interested parties are given maximum opportunity to share their views.” The coalition has been conducting public information sessions, including one in Mansfield this week, to provide state residents with information on "what the proposed health care mergers will mean for Connecticut consumers."
A week ago, State Comptroller Kevin Lembo, in a letter to the Department, urged an open and thorough review in order to address significant concerns raised by health care consumers and providers. Lembo expressed his support for the efforts of the Connecticut Campaign for Consumer Choice, noting that a merger between Anthem and Cigna would increase the Connecticut health insurance concentration over 40 percent. Lembo indicated that only Georgia is expected to experience a more significant increase in market concentration.
CIGNA Questions Anthem; Feds Question CIGNA
A week ago, Modern Healthcare, a web publication focused on healthcare business news, raised questions about the absence of detail in the year since Anthem disclosed “what was by far the largest data breach in healthcare history. The cyberattack—in which hackers stole the names, birth dates, Social Security numbers, home addresses and other personal information of 78.8 million current and former members and employees – caused consumers to question “whether Anthem and other healthcare organizations could manage the volumes of data they had,” according to the news report. 
The publication also questioned whether state regulators would consider not only the breach, but CIGNA’s reaction to it at the time:
“Trust with customers and providers is critical in our industry, and Anthem has yet to demonstrate a path towards restoring this trust,” CIGNA CEO David Cordani and former Board Chairman Isaiah Harris Jr. wrote in a June 21, 2015 letter: “We need to understand the litigation and potential liabilities, operational impact and long-term damage to Anthem's franchise as a result of this unprecedented data breach, as well as the governance and controls that resulted in this system failure.” It was estimated that in Connecticut, about 1.7 million people were affected.
In January, published reports indicated that U.S. regulators temporarily banned CIGNA-HealthSpring from offering certain Medicare plans to new patients after a probe uncovered issues with current offerings, citing that CIGNA’s deficiencies “Create a Serious Threat to Enrollee Health and Safety.” CIGNA disclosed that the U.S. Centers for Medicare and Medicaid Services (CMS) had suspended the company from enrolling new customers or marketing plans for CIGNA Medicare Advantage and Standalone Prescription Drug Plan Contracts. CIGNA acquired HealthSpring in 2012.
In an enforcement letter, CMS accused CIGNA of "widespread and systemic failures," including the denial of health care coverage and prescription drugs to patients who should have received them. The actions "create a serious threat to enrollee health and safety," said CMS, which required CIGNA to appoint an independent monitor to audit its handling of the matter.
“Cigna has had a longstanding history of non-compliance with CMS requirements. Cigna has received numerous notices of non-compliance, warning letters, and corrective action plans from CMS over the past several years. A number of these notices were for the same violations discovered during the audit, demonstrating that Cigna has not corrected issues of non-compliance,” said the 12-page enforcement letter from the Director of the Medicare Parts C and D Oversight and Enforcement Group.
CIGNA, First in Connecticut
Nearly five years ago, in July 2011, CIGNA announced it was to receive $50 million in economic benefits from the Connecticut Department of Economic and Community Development with the promise of adding at least 200 jobs the following two years, which would increase the company’s employment in the state to more than 4,000. CIGNA also declared Bloomfield its corporate headquarters in the United States, replacing Philadelphia which had been the company’s corporate headquarters since 1982.
CIGNA was the first company to receive economic incentives under Governor Dannel Malloy’s “First Five” program, which was designed to spur job growth and support Connecticut businesses in becoming more competitive in the global marketplace. “CIGNA is proof that these tools work and that Connecticut is open for business,” Malloy said at the time.
“Through this partnership with the Governor and the state, we are building upon our long history in Connecticut,” added CIGNA Chief Executive Officer David Cordani.
Anthem's application states it has "no current plans or proposals to reduce in any material respect the number of employees employed by the Cigna companies." The $54 billion merger would increase Anthem's membership from 38 million to 53 million members nationwide.
Approval in Florida, Concerns in California
“There are no meaningful adverse impacts resulting from the acquisition,” Florida’s Insurance Commissioner said last week in approving the acquisition in his state. “The companies, individually or in combination, are an important part of, but not a dominant factor in, the Florida market, and their combination does not noticeably increase the market concentration across the broadly measured market on a statewide basis.”
In California, the combined membership of Anthem Blue Cross and Cigna would make it the largest insurer in the state with more than 8 million members. At a public hearing in California last month convened by that state’s Insurance Department, consumer advocates and the AMA opposed the acquisition.
"This merger would create the nation's largest insurer, which could have a significant impact on California's consumers, businesses, and the healthcare marketplace," said California’s Insurance Commissioner. "I am considering what is best for consumers and the overall marketplace. Anthem and Cigna bear the burden of demonstrating this proposed merger is in the best interest of California consumers and the health-care marketplace."
Shareholders of Anthem and Cigna voted overwhelmingly in favor of the merger plan late last year, and regulators in 26 states where the companies operate are at various stages of considering the acquisition. Attorneys General in a number of those states, including Connecticut, are looking into the proposed acquisition on anti-trust grounds, and the U.S. Department of Justice has the final authority to approve the deal, published reports indicate.
The news site Business Insurance reported soon after the acquisition was announced that “viewed in tandem with rival Aetna Inc.'s recent $37 billion merger agreement with Humana Inc.— as well as St. Louis-based health insurer Centene Corp.'s proposed acquisition of Woodland Hills, California-based Health Net Inc. for $6.3 billion — experts said regulators may be more stringent in examining the Anthem/Cigna deal's potential to dampen health insurer competition.”
 Quality of life in the United States is heavily dependent on financial status, the survey summary points out. As a consequence, the nation’s best states to live in often report very high incomes. With a median household income of $71,346 a year, fifth highest of all states, Connecticut is the second best state to live in and an especially good example of this pattern, the description of Connecticut’s ranking explains.
Quality of life in the United States is heavily dependent on financial status, the survey summary points out. As a consequence, the nation’s best states to live in often report very high incomes. With a median household income of $71,346 a year, fifth highest of all states, Connecticut is the second best state to live in and an especially good example of this pattern, the description of Connecticut’s ranking explains.

 “Any member of the public interested in the proposed acquisition of control may attend the hearing,” indicates a public notice of the hearing. In addition, “Any policyholder of Cigna HealthCare of Indiana, Inc., or other person whose interests may be affected by the proposed acquisition of control shall have the right to appear and become party to the proceeding.”
“Any member of the public interested in the proposed acquisition of control may attend the hearing,” indicates a public notice of the hearing. In addition, “Any policyholder of Cigna HealthCare of Indiana, Inc., or other person whose interests may be affected by the proposed acquisition of control shall have the right to appear and become party to the proceeding.”



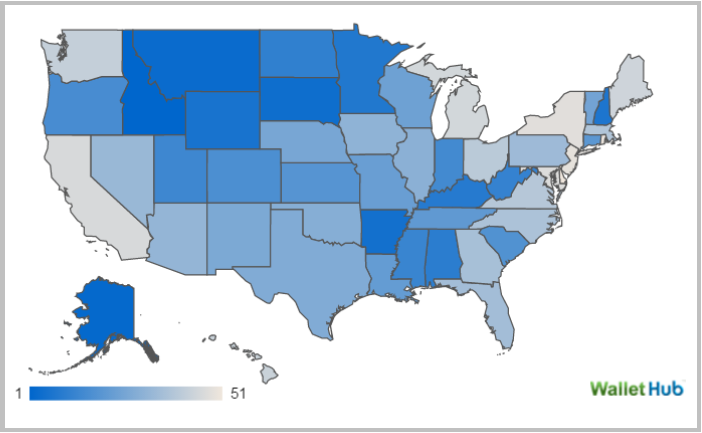
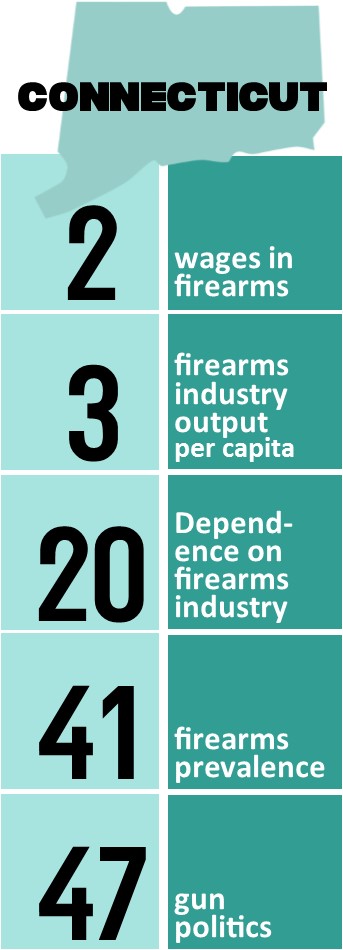 With the gun debate center-stage in the presidential primaries and in Washington, D.C., the website WalletHub analyzed which states depend most on the arms and ammunitions industry both directly for jobs and political contributions and indirectly through firearm ownership. WalletHub’s analysts compared the 50 states and the District of Columbia across three key dimensions: 1) Firearms Industry, 2) Gun Prevalence and 3) Gun Politics and eight metrics.
With the gun debate center-stage in the presidential primaries and in Washington, D.C., the website WalletHub analyzed which states depend most on the arms and ammunitions industry both directly for jobs and political contributions and indirectly through firearm ownership. WalletHub’s analysts compared the 50 states and the District of Columbia across three key dimensions: 1) Firearms Industry, 2) Gun Prevalence and 3) Gun Politics and eight metrics.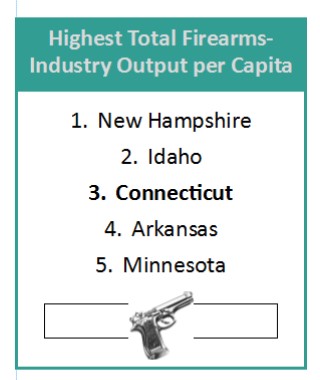
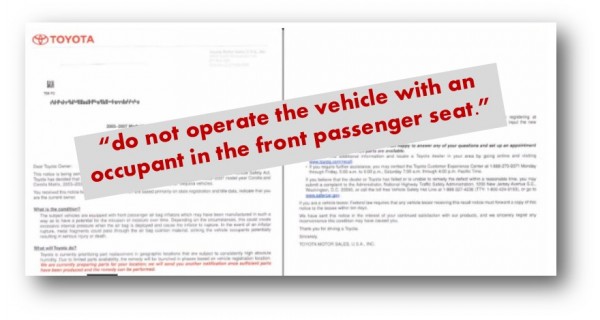

 The company, and impacted automakers, are making parts necessary to accomplish repairs available in regions of the country with humid climates first, because humidity has been said to increase the risk of air bag rupture. Connecticut residents, living in a region not known for its humidity, are not a priority for the repair, and continue to wait for word when repairs for their recalled vehicles can be made.
The company, and impacted automakers, are making parts necessary to accomplish repairs available in regions of the country with humid climates first, because humidity has been said to increase the risk of air bag rupture. Connecticut residents, living in a region not known for its humidity, are not a priority for the repair, and continue to wait for word when repairs for their recalled vehicles can be made.





 6.8 million employees in all, more than ever, according to Fortune, whose issue with the 61st annual ranking is out this week.
6.8 million employees in all, more than ever, according to Fortune, whose issue with the 61st annual ranking is out this week. One of the two new entries on this year’s list that are headquartered in Connecticut is
One of the two new entries on this year’s list that are headquartered in Connecticut is 
 Amphenol World Headquarters
Amphenol World Headquarters



 w your firm to freely innovate, grow, and prosper.”
w your firm to freely innovate, grow, and prosper.”
 The website recalls that “in Connecticut, Governor Ella Grasso was trying to drive from the Governor’s Mansion to the state storm center in downtown H
The website recalls that “in Connecticut, Governor Ella Grasso was trying to drive from the Governor’s Mansion to the state storm center in downtown H artford. She didn’t quite make it. Forced to abandon her car and walk the remaining blocks to the state armory, Grasso was not slow in taking the storm seriously. Thanks to (Massachusetts Governor Michael) Dukakis and Grasso, both state and National Guard troops would soon be on their way.”
artford. She didn’t quite make it. Forced to abandon her car and walk the remaining blocks to the state armory, Grasso was not slow in taking the storm seriously. Thanks to (Massachusetts Governor Michael) Dukakis and Grasso, both state and National Guard troops would soon be on their way.”