CT Office of Early Childhood Receives Global Recognition for Effective Communication
/The Connecticut Office of Early Childhood (OEC) – a state agency that didn’t exist just over five years ago - has earned global recognition for success and innovation in serving the state’s youngest children and their families. The agency was chosen to receive the “Future of Feedback Award” at the annual Feedback Summit in Washington, D.C. The award was presented last week to OEC Commissioner David Wilkinson for his agency’s efforts at effective listening to the people it serves and the nonprofit providers who serve them.
“The Office of Early Childhood is honored to be recognized for its efforts in communicating effectively with Connecticut’s families and providers, and for finding strategies to meet their needs,” said Commissioner Wilkinson. “The parents we serve and the community providers we support are the best experts in what they need to succeed, but too often they don’t have a seat at the table. OEC is trying a new approach to put parents and our hardworking providers at the center of our policymaking. We’re saying, ‘nothing we plan for you should be done without you.’’
"Connecticut’s Office of Early Childhood is pioneering innovative ways of both listening and acting. OEC’s outreach to families – and frontline service providers – is creating conversations about what matters most, and what they can all do together," said Dennis Whittle, Co-Founder of Feedback Labs and GlobalGiving.
Feedback Labs, the organizer of the Summit, is a global network of over 400 leading aid, philanthropy, and governance organizations around the world. Feedback Labs was conceived in 2013 and launched in connection with the Obama White House. Whittle also co-founded GlobalGiving, a leading marketplace connecting social, environmental, and economic development projects to individual and corporate donors. Since its inception GlobalGiving has facilitated $335 million in funding to over 20,000 projects in 170 countries.
Established in 2014 through a bipartisan effort of Gov. Dannel Malloy and the legislature, OEC oversees and funds Connecticut’s early childhood programming – including child care, pre-K, early intervention for children with developmental delays, and family support services for at risk families – components that once were housed in five disparate state agencies.
 Among the 10 largest state agencies in Connecticut, OEC’s goal is to keep the state’s children safe, healthy, learning and thriving. Through its innovative feedback efforts, the agency is acting on evidence that engaging providers and parents in policymaking yields better results. Officials said that the agency combined data from 1,700 family surveys, another survey shared with all providers in the state, and 400 community and provider meetings in order to build a draft plan to transform the ECE system in the state, which serves 200,000 children.
Among the 10 largest state agencies in Connecticut, OEC’s goal is to keep the state’s children safe, healthy, learning and thriving. Through its innovative feedback efforts, the agency is acting on evidence that engaging providers and parents in policymaking yields better results. Officials said that the agency combined data from 1,700 family surveys, another survey shared with all providers in the state, and 400 community and provider meetings in order to build a draft plan to transform the ECE system in the state, which serves 200,000 children.
Wilkinson added that “An award like this is an encouraging validation of our efforts to listen to families and providers, and then do all we can to act on their advice. We believe that by listening and responding, we will provide better, more effective services for Connecticut families with young children – and in so doing help create a brighter future for the state.”
"OEC’s approach contains key ingredients of more responsive, innovative, and effective government. OEC’s leadership in asking for and responding to feedback has the potential to spread widely through the public sector,” Whittle added.
“Child care centers work hard every day for children,” Said Dr. Monette Ferguson, Executive Director of ABCD, Inc., a nonprofit operating several leading child care centers in and around Bridgeport. “Usually the state tells us what to do and by the time we share any concerns, it’s too late. I am not used to a state agency asking what I think before it acts. It’s good to feel heard and to see OEC acting on our advice.”
David Wilkinson was named Commissioner by Gov. Malloy in April 2017 to serve as the second Commissioner of the state’s Office of Early Childhood (OEC). He previously served as Director of the White House Office of Social Innovation and Civic Participation under President Barack Obama. While at the White House, Wilkinson worked closely with the Malloy Administration on signature early childhood efforts, including a first-of-its-kind initiative – scaling a program proven to reduce parental substance use and child welfare interaction – for which the administration has achieved national acclaim. He has also served as an advisor to the Yale Child Study Center, a leading collaborator with the state and its early childhood service providers.
Christine Johnson-Staub is the Interim Director of Child Care and Early Education at CLASP, a 50-year-old national nonprofit based in Washington, D.C., that focuses on shaping policy to support families living in poverty. She said, “OEC’s approach to setting its policy direction was unique because not only did it build on input from the community and existing research and data, but it went back to a wide range of impacted people, including parents, providers and other stakeholders, to make sure they got it right.”
“Parents and child care providers know the challenges facing the early care system better than anyone but rarely does anyone from state government ask our opinion,” said Merrill Gay, Executive Director of the nonprofit Early Childhood Alliance, a state consortium of providers and advocates. “That's why it was so refreshing to have the Office of Early Childhood ask us: ‘What are the pain points? How do we make this system work better for you?’ I'm really excited to see OEC now turning that agenda for improvement into concrete action to better serve children and families.”
The strategy of communicating successfully with a target audience, and then acting upon that communication, is known as a “feedback loop” – an approach widely studied and increasingly appreciated by thought leaders, initially gaining traction in international development, but seen to have powerful implications for advancing more responsive, cost-effective and impactful government services in the US. The 2018 Feedback Summit was attended by over 150 feedback pioneers and leaders from around the U.S. and the world.
“They speak. We listen. We make change. It’s about being responsive to the needs of the young children in our state and, of course, their parents and caregivers,” Wilkinson said. To contact the Office of Early Childhood, visit www.ct.gov/oec or call (860) 500-4412.


 To assist patients who find themselves in this difficult situation, several states have passed legislation mandating a limit on out-of-pocket costs for medications. These limits can be applied in different forms, such as a per-drug cap or by mandating a copay-only structure in certain health plans. Those are just some of the areas of particular interest to
To assist patients who find themselves in this difficult situation, several states have passed legislation mandating a limit on out-of-pocket costs for medications. These limits can be applied in different forms, such as a per-drug cap or by mandating a copay-only structure in certain health plans. Those are just some of the areas of particular interest to 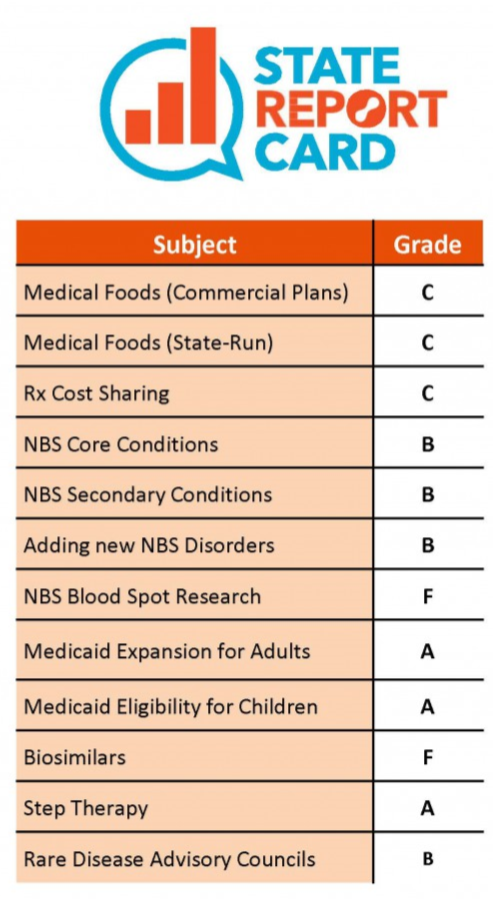


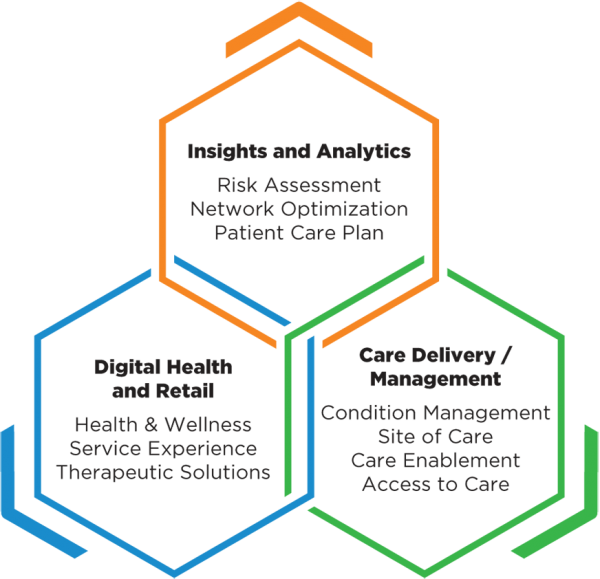 Companies in the portfolio, according to published reports, include Omada Health, a digital therapeutics company treating chronic diseases; Prognos, a predictive analytics company for healthcare; Contessa Health, a home-patient care service; Mdlive, which provides remote health consultations; and Cricket Health, a special kidney care provider.
Companies in the portfolio, according to published reports, include Omada Health, a digital therapeutics company treating chronic diseases; Prognos, a predictive analytics company for healthcare; Contessa Health, a home-patient care service; Mdlive, which provides remote health consultations; and Cricket Health, a special kidney care provider.

 Obesity is a problem in virtually every city and town, and every income and social sector. But its impact is most serious in communities where conditions make access to healthy foods and regular physical activity more difficult, such as lower income and rural areas, including many communities of color. The national costs of obesity are enormous, officials point out. Obesity drives an estimated $149 billion annually in directly related healthcare spending, and an additional $66 billion annually in lowered economic productivity. Also, one in three young adults is ineligible for military service, due to being overweight, officials noted.
Obesity is a problem in virtually every city and town, and every income and social sector. But its impact is most serious in communities where conditions make access to healthy foods and regular physical activity more difficult, such as lower income and rural areas, including many communities of color. The national costs of obesity are enormous, officials point out. Obesity drives an estimated $149 billion annually in directly related healthcare spending, and an additional $66 billion annually in lowered economic productivity. Also, one in three young adults is ineligible for military service, due to being overweight, officials noted.
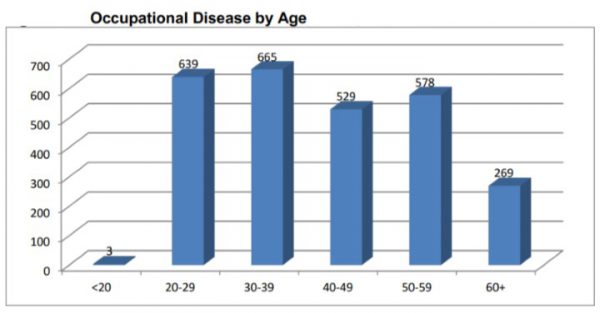
 Among the report’s other key findings:
Among the report’s other key findings: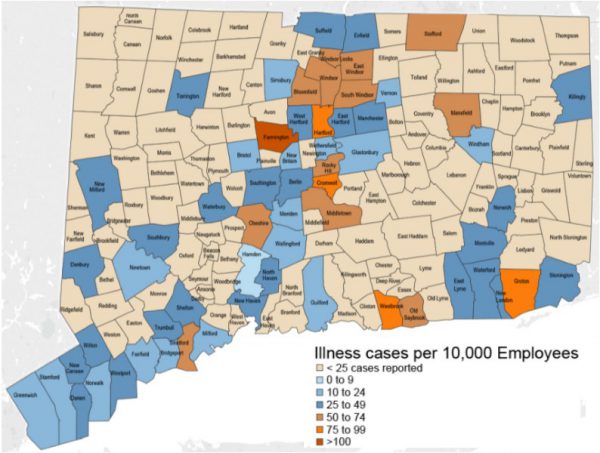
 These higher town rates often reflect the locations of large employers in higher hazard industries, and may also reflect better reporting of cases, since cases of occupational illness are often not reported, the study points out.
These higher town rates often reflect the locations of large employers in higher hazard industries, and may also reflect better reporting of cases, since cases of occupational illness are often not reported, the study points out.

 Pagoto is also Director of the UConn Center for mHealth and Social Media. She is also a licensed clinical psychologist her research focuses on leveraging technology in the development and delivery of behavioral interventions targeting diet, physical activity, and cancer prevention behaviors. She has had federal funding for her program of research for 14 consecutive years, totaling over $11 million, and has published over 170 papers in peer-reviewed journals, according to the UConn website.
Pagoto is also Director of the UConn Center for mHealth and Social Media. She is also a licensed clinical psychologist her research focuses on leveraging technology in the development and delivery of behavioral interventions targeting diet, physical activity, and cancer prevention behaviors. She has had federal funding for her program of research for 14 consecutive years, totaling over $11 million, and has published over 170 papers in peer-reviewed journals, according to the UConn website. Atop the rankings in the pediatric specialty were Children’s National Medical Center (Washington, DC), Children’s Hospital of Philadelphia, Boston Children’s Hospital, Children’s Hospital Colorado, Cincinnati Children’s Hospital Medical Center, Rainbow Babies and Children’s Hospital (Cleveland), UCSF Benioff Children’s Hospital of San Francisco and Oakland, New York-Presbyterian Morgan Stanley-Komansky Children’s Hospital, St. Louis Children’s Hospital-Washington University, and C.S. Mott Children’s Hospital – Michigan Medicine (Ann Arbor).
Atop the rankings in the pediatric specialty were Children’s National Medical Center (Washington, DC), Children’s Hospital of Philadelphia, Boston Children’s Hospital, Children’s Hospital Colorado, Cincinnati Children’s Hospital Medical Center, Rainbow Babies and Children’s Hospital (Cleveland), UCSF Benioff Children’s Hospital of San Francisco and Oakland, New York-Presbyterian Morgan Stanley-Komansky Children’s Hospital, St. Louis Children’s Hospital-Washington University, and C.S. Mott Children’s Hospital – Michigan Medicine (Ann Arbor). e, infection rates in the NICU and other data collected from a detailed U.S. News clinical survey of children's hospitals, produced 85 percent of each hospital's score. The other 15 percent reflects nominations from pediatric specialists and subspecialists who responded to surveys in 2016, 2017 and 2018 and recommended the hospital for serious cases in their specialty.
e, infection rates in the NICU and other data collected from a detailed U.S. News clinical survey of children's hospitals, produced 85 percent of each hospital's score. The other 15 percent reflects nominations from pediatric specialists and subspecialists who responded to surveys in 2016, 2017 and 2018 and recommended the hospital for serious cases in their specialty.