Suicide Numbers Increasing; Efforts Intensify to Respond, Prevent
/The Centers for Disease Control and Prevention (CDC) released a report this year that suicide rates nationally jumped by 25 percent since 1999, a finding that “shocked” even experts who believed the rate had been flat. Each year, more than 41,000 individuals die by suicide, leaving behind their friends and family members to navigate the tragedy of loss, according to the National Alliance on Mental Illness. Connecticut's rate, 9.7 deaths per 100,000, rose 20 percent during that time, and 49 states saw an increase, according to the CDC. Connecticut’s suicide rate, is ranked number 46 in the country.
Suicide is the 10th leading cause of death in the U.S. with one occurring on average every 13.3 minutes. September is National Suicide Prevention Month.
For every suicide, there are 30 people who made the attempt, Dr. James F. O'Dea, vice president of the Behavior Health Network of Hartford Healthcare, recently told the Meriden Record-Journal. The U.S. Health Resources & Services Administration reports that “approximately 45% of suicide victims had contact with primary care providers within 1 month of suicide.”

“Connecticut suicide rates may have not have increased as much in comparison to other states, but isn’t the real question, ‘Why is it increasing at all?’” Luis Perez, president and CEO of Mental Health Connecticut, told The Hartford Courant earlier this year.
“It’s been well-researched that most people who die by suicide do so because they want the pain to stop — and they don’t see any other way,” Perez said. “Prevention is critical. Knowing the safe and right way to talk to someone who may have thoughts of suicide and letting people know they are not alone, that millions of people struggle with suicide ideation is key.”
According to the state Department of Public Health, approximately 31 percent of victims had a history of treatment for mental illness and 42 percent had previously attempted or thought about suicide or disclosed their intent to commit suicide. The CDC offers 5 steps to help someone at risk: 1. Ask. 2. Keep them safe. 3. Be there. 4. Help them connect. 5. Follow up.
The U.S. government’s anti-bullying website, stopbullying.com, points out that “many issues contribute to suicide risk, including depression, problems at home, and trauma history. Additionally, specific groups have an increased risk of suicide, including American Indian and Alaskan Native, Asian American, lesbian, gay, bisexual, and transgender youth.” The site indicates that “this risk can be increased further when these kids are not supported by parents, peers, and schools. Bullying can make an unsupportive situation worse.”
Matt Riley, Chief Operating Officer of the Connecticut-based Jordan Porco Foundation, recently told WTNH-TV that suicide is the second leading cause of death for Americans ages 15 to 24. One in ten college students and one in five high school students consider suicide. Young people considering suicide are most likely to talk to peers, so the Jordan Porco Foundation focuses on peer-to-peer outreach and awareness, with a series of successful program initiatives on college campuses in Connecticut and across the country.
In recent years, a new student-driven primary prevention program was piloted to help high school students develop positive coping skills and enhance protective factors in preparation for life beyond high school. Schools and organizations participating included Manchester High School, Immaculate High School in Danbury, Enfield Public Schools, Capital Preparatory High School in Hartford, Institute of Living in Hartford, Jewish Family Services in West Hartford, Wilton High School, Boys & Girls Club of Bristol, and Guilford Youth & Family Services.
Numerous organizations across Connecticut offer Mental Health First Aid, an 8-hour training to teach participants how to help someone who is developing a mental health problem or experiencing a mental health crisis. The evidence behind the program demonstrates that it helps trainees identify, understand and respond to signs of mental illnesses and substance use disorders. The course is often offered to participants free of charge.
https://youtu.be/TT_HLG5FkKA
https://youtu.be/jl87bmuCTdM



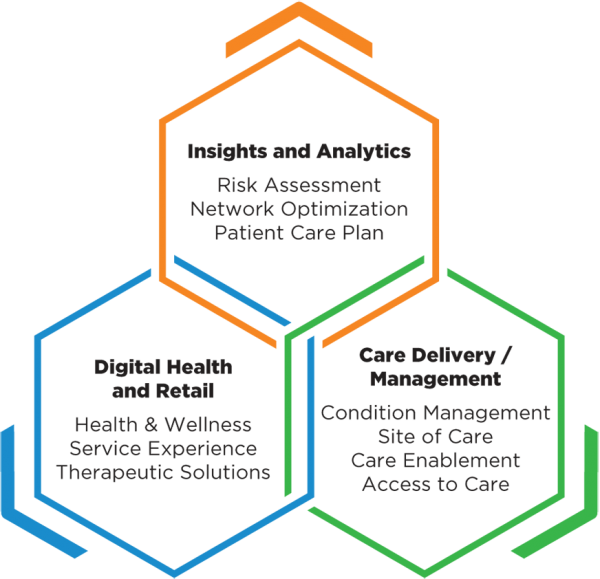 Companies in the portfolio, according to published reports, include Omada Health, a digital therapeutics company treating chronic diseases; Prognos, a predictive analytics company for healthcare; Contessa Health, a home-patient care service; Mdlive, which provides remote health consultations; and Cricket Health, a special kidney care provider.
Companies in the portfolio, according to published reports, include Omada Health, a digital therapeutics company treating chronic diseases; Prognos, a predictive analytics company for healthcare; Contessa Health, a home-patient care service; Mdlive, which provides remote health consultations; and Cricket Health, a special kidney care provider.

 Obesity is a problem in virtually every city and town, and every income and social sector. But its impact is most serious in communities where conditions make access to healthy foods and regular physical activity more difficult, such as lower income and rural areas, including many communities of color. The national costs of obesity are enormous, officials point out. Obesity drives an estimated $149 billion annually in directly related healthcare spending, and an additional $66 billion annually in lowered economic productivity. Also, one in three young adults is ineligible for military service, due to being overweight, officials noted.
Obesity is a problem in virtually every city and town, and every income and social sector. But its impact is most serious in communities where conditions make access to healthy foods and regular physical activity more difficult, such as lower income and rural areas, including many communities of color. The national costs of obesity are enormous, officials point out. Obesity drives an estimated $149 billion annually in directly related healthcare spending, and an additional $66 billion annually in lowered economic productivity. Also, one in three young adults is ineligible for military service, due to being overweight, officials noted.
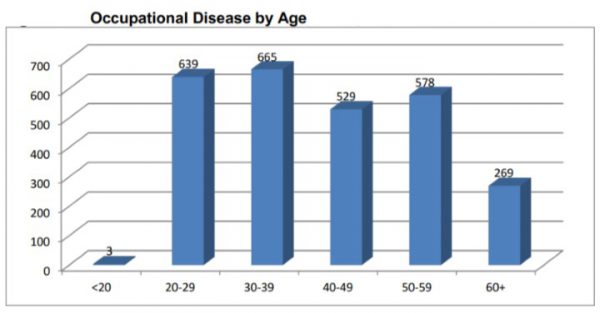
 Among the report’s other key findings:
Among the report’s other key findings: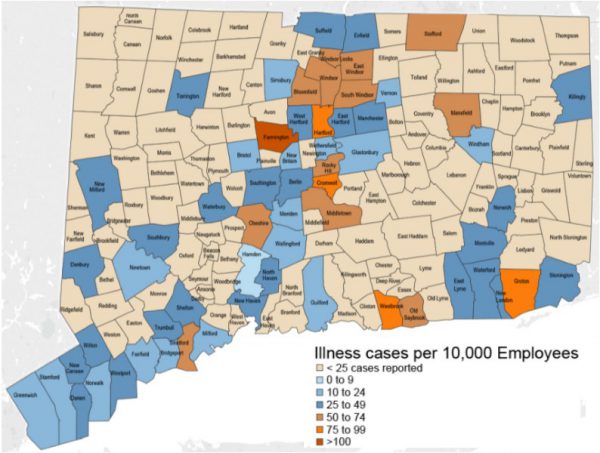
 These higher town rates often reflect the locations of large employers in higher hazard industries, and may also reflect better reporting of cases, since cases of occupational illness are often not reported, the study points out.
These higher town rates often reflect the locations of large employers in higher hazard industries, and may also reflect better reporting of cases, since cases of occupational illness are often not reported, the study points out.

 Pagoto is also Director of the UConn Center for mHealth and Social Media. She is also a licensed clinical psychologist her research focuses on leveraging technology in the development and delivery of behavioral interventions targeting diet, physical activity, and cancer prevention behaviors. She has had federal funding for her program of research for 14 consecutive years, totaling over $11 million, and has published over 170 papers in peer-reviewed journals, according to the UConn website.
Pagoto is also Director of the UConn Center for mHealth and Social Media. She is also a licensed clinical psychologist her research focuses on leveraging technology in the development and delivery of behavioral interventions targeting diet, physical activity, and cancer prevention behaviors. She has had federal funding for her program of research for 14 consecutive years, totaling over $11 million, and has published over 170 papers in peer-reviewed journals, according to the UConn website. Atop the rankings in the pediatric specialty were Children’s National Medical Center (Washington, DC), Children’s Hospital of Philadelphia, Boston Children’s Hospital, Children’s Hospital Colorado, Cincinnati Children’s Hospital Medical Center, Rainbow Babies and Children’s Hospital (Cleveland), UCSF Benioff Children’s Hospital of San Francisco and Oakland, New York-Presbyterian Morgan Stanley-Komansky Children’s Hospital, St. Louis Children’s Hospital-Washington University, and C.S. Mott Children’s Hospital – Michigan Medicine (Ann Arbor).
Atop the rankings in the pediatric specialty were Children’s National Medical Center (Washington, DC), Children’s Hospital of Philadelphia, Boston Children’s Hospital, Children’s Hospital Colorado, Cincinnati Children’s Hospital Medical Center, Rainbow Babies and Children’s Hospital (Cleveland), UCSF Benioff Children’s Hospital of San Francisco and Oakland, New York-Presbyterian Morgan Stanley-Komansky Children’s Hospital, St. Louis Children’s Hospital-Washington University, and C.S. Mott Children’s Hospital – Michigan Medicine (Ann Arbor). e, infection rates in the NICU and other data collected from a detailed U.S. News clinical survey of children's hospitals, produced 85 percent of each hospital's score. The other 15 percent reflects nominations from pediatric specialists and subspecialists who responded to surveys in 2016, 2017 and 2018 and recommended the hospital for serious cases in their specialty.
e, infection rates in the NICU and other data collected from a detailed U.S. News clinical survey of children's hospitals, produced 85 percent of each hospital's score. The other 15 percent reflects nominations from pediatric specialists and subspecialists who responded to surveys in 2016, 2017 and 2018 and recommended the hospital for serious cases in their specialty.





 According to the Nature Conservancy, Bridgeport currently has a 19% tree canopy cover, for example. If all open spaces, vacant lots and parking lots could be planted, the city would have a 62% tree canopy cover. The ramifications would be substantial, impacting various health and quality of life factors.
According to the Nature Conservancy, Bridgeport currently has a 19% tree canopy cover, for example. If all open spaces, vacant lots and parking lots could be planted, the city would have a 62% tree canopy cover. The ramifications would be substantial, impacting various health and quality of life factors.


























