How Does Your Health Insurance Plan Stack Up? There’s A Resource for That
/Connecticut’s Insurance Department has issued its 2018 Consumer Report Card on Health Plans in Connecticut, providing consumers with an updated snapshot of 12 health carriers in the Connecticut marketplace. The goal: to help consumers make informed choices when choosing a health plan.
“The Department’s annual Report Card is designed to deliver side-by-side comparisons of health carriers across a variety of quality measures, including coverage for mental health and substance abuse treatment,” Commissioner Katharine L. Wade said recently. The analysis includes health claims, mental healthcare, pregnancy coverage and preventative care, and reviews the reasons cited in instances of denial of coverage. 
Among the trends identified in the latest annual report care are:
- Total enrollment over 2.2 million, a slight increase from 2016.
- 5 percent of those covered (1.85 million people) get their insurance from large group plans
- 131,000 people have individual plans (5.9 percent)
- 235,000 people are covered under small group plans (10.6 percent)
The 72-page data-filled report card also notes that there was an increase in the number of primary care providers, specialists and pharmacies participating in health plan networks. There was a decline in the number of participating hospitals, officials indicated, but attributed it “primarily due to consolidations in the industry and not facilities closing.”
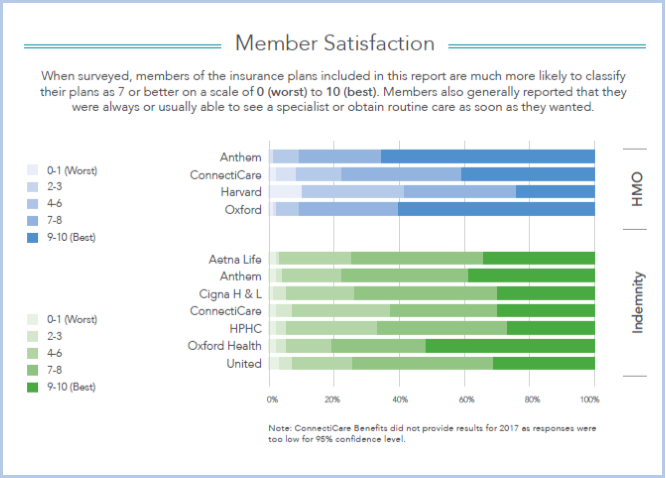
Customers surveyed said they were always or usually able to see a specialist or get routine care as soon as they wanted. The enrollment breakdown in Connecticut is lopsided. Among HMO's, Anthem has 81% of the market, ConnectiCare 17%, Oxford 2%. Among indemnity enrollments, Anthem has 42%, followed by Aetna's 20%, CIGNA's 19%, United's 7% and ConnectiCare's 5%.
The report card, issued this fall, includes “terms” that consumers should know, a series of frequently asked questions and answers, and results of a member satisfaction survey for HMO’s Anthem, ConnectiCare, Harvard Pilgrim and Oxford Health. Indemnity insurers Aetna Life, Anthem, CIGNA, ConnectiCare, Harvard Pilgrim, United Health and Oxford Health also had members surveyed on a range of “satisfaction” queries.
This report includes three years of data, where available, to be informative for consumers, officials said. The data utilized was through 2017.
The mission of the Connecticut Insurance Department is to protect consumers through regulation of the industry, outreach, education and advocacy. The Department recovers an average of $4 million yearly on behalf of consumers, according to officials, and regulates the industry by ensuring carriers adhere to state insurance laws and regulations and are financially solvent to pay claims.
Each year, the Department returns an average of $100 million a year to the state General Fund in license fees, premium taxes, fines and other revenue sources to support various state programs, including childhood immunization. The Department’s annual budget is funded through assessments from the insurance industry.
Individuals with questions or seeking further information may contact the Department at insurance@ct.gov or 860-297-3900.


 The state
The state 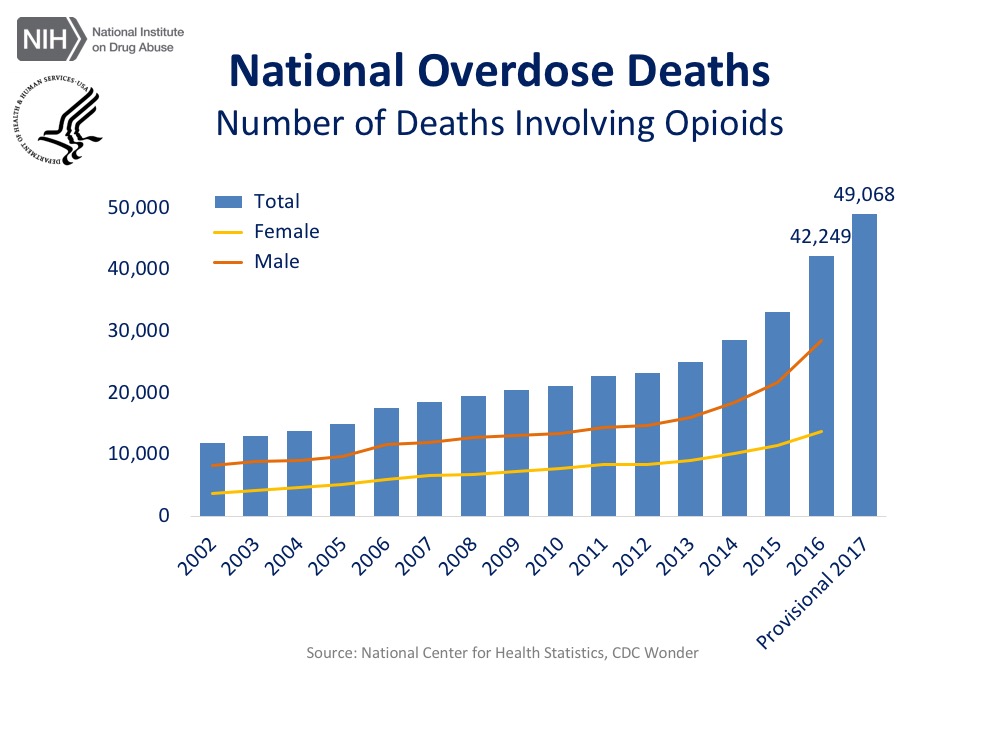

 t have increased as much in comparison to other states, but isn’t the real question, ‘Why is it increasing at all?’” Luis Perez, president and CEO of
t have increased as much in comparison to other states, but isn’t the real question, ‘Why is it increasing at all?’” Luis Perez, president and CEO of  The analysis, by the financial services website WalletHub, was based on 40 key indicators of livability, ranging from housing costs to school-system quality to restaurants per capita. The indicators were grouped into five categories – affordability, economic health, education & health, safety, and quality of life.
The analysis, by the financial services website WalletHub, was based on 40 key indicators of livability, ranging from housing costs to school-system quality to restaurants per capita. The indicators were grouped into five categories – affordability, economic health, education & health, safety, and quality of life.
 The survey revealed that residents are not satisfied with the current health care system: 80 percent agree or strongly agree that “the system needs to change.” When given more than 20 options, they focused on the high prices charged by industry players, citing most frequently as a “major reason” for high health care costs:
The survey revealed that residents are not satisfied with the current health care system: 80 percent agree or strongly agree that “the system needs to change.” When given more than 20 options, they focused on the high prices charged by industry players, citing most frequently as a “major reason” for high health care costs:
 The 40-page report, developed by The Child Health and Development Institute of Connecticut (CHDI), a subsidiary of the Children’s Fund of Connecticut, in partnership with the national Center for School Mental Health at the University of Maryland, provides a framework for policymakers and school districts interested in improving outcomes by addressing the mental health and trauma needs of students. The report indicates that “in a typical classroom of 25 students, approximately five will meet criteria for a mental health disorder but most of them are not receiving appropriate mental health treatment or support. Among those who do access care, approximately 70 percent receive services through their schools.”
The 40-page report, developed by The Child Health and Development Institute of Connecticut (CHDI), a subsidiary of the Children’s Fund of Connecticut, in partnership with the national Center for School Mental Health at the University of Maryland, provides a framework for policymakers and school districts interested in improving outcomes by addressing the mental health and trauma needs of students. The report indicates that “in a typical classroom of 25 students, approximately five will meet criteria for a mental health disorder but most of them are not receiving appropriate mental health treatment or support. Among those who do access care, approximately 70 percent receive services through their schools.” “Approaching student mental health with a comprehensive lens that integrates health promotion, prevention, early intervention, and more intensive treatments leads to better school, student and community outcomes," said Dr. Sharon Hoover, Co-Director of the Center for School Mental Health at the University of Maryland and lead author of the report.
“Approaching student mental health with a comprehensive lens that integrates health promotion, prevention, early intervention, and more intensive treatments leads to better school, student and community outcomes," said Dr. Sharon Hoover, Co-Director of the Center for School Mental Health at the University of Maryland and lead author of the report.
 The personal-finance website WalletHub compared the largest U.S. cities – including at least two from each state - across 31 key indicators of disability-friendliness. The data set ranges from wheelchair-accessible facilities per capita to rate of workers with disabilities to quality of public hospital system. The 31 indicators were grouped into three categories: Economy, Quality of Life and Health Care.
The personal-finance website WalletHub compared the largest U.S. cities – including at least two from each state - across 31 key indicators of disability-friendliness. The data set ranges from wheelchair-accessible facilities per capita to rate of workers with disabilities to quality of public hospital system. The 31 indicators were grouped into three categories: Economy, Quality of Life and Health Care.
 “Bridgeport has one of the lowest number of wheelchair accessible art, entertainment and recreational establishments per capita, and a large number of older buildings with little to no access for disabled residents," Gonzalez said.
“Bridgeport has one of the lowest number of wheelchair accessible art, entertainment and recreational establishments per capita, and a large number of older buildings with little to no access for disabled residents," Gonzalez said.